Quick version
Multidrug-resistant E. coli strains pose a serious threat to public health. By maintaining good hygiene, handling food safely, and using antibiotics responsibly, we can all contribute to slowing the spread. At the same time, continued research and international collaboration are essential to address this growing crisis.
According to the Swedish Public Health Agency, a multidrug-resistant strain of *E. coli* has become established in Europe and has also spread to Sweden. This bacterium is resistant to several common treatment options, including broad-spectrum antibiotics such as carbapenems.
Over 300 cases have been identified in Sweden in 2024, representing a significant increase compared to the previous year. The Swedish Public Health Agency is closely monitoring the development of cases and characterizing all findings to detect and prevent national spread, as well as tracking changes in resistance mechanisms and patterns.
SourcesEuropean Centre for Disease Prevention and Control (ECDC): Antibiotic Resistance.
World Health Organization (WHO): Antimicrobial Resistance.
Swedish Food Agency: Food safety and foodborne illness guidelines.
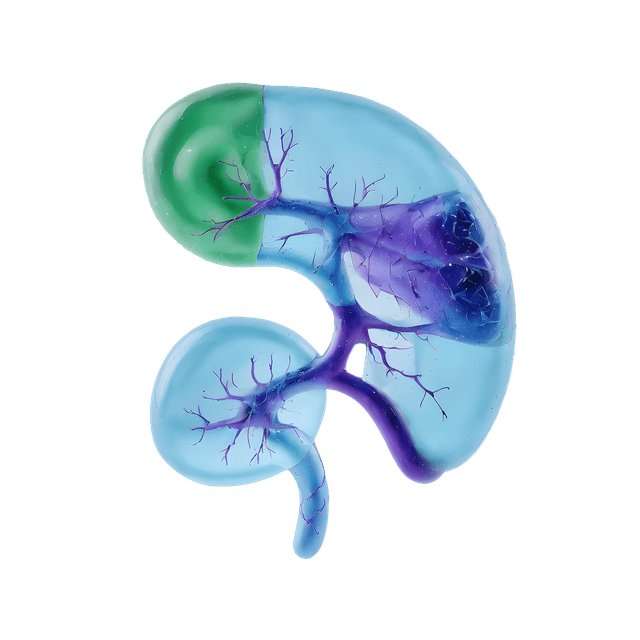
What makes the E. coli bacterium a particular threat right now?
A multidrug-resistant strain of Escherichia coli poses a particular threat because it is resistant to several antibiotics traditionally used to treat infections. This means that infections such as urinary tract infections, abdominal infections, or bloodstream infections can no longer be effectively treated with standard medications. When antibiotics fail, extensive laboratory analyses are required to determine which, if any, antibiotics might be effective.
How E. coli spreads
The multidrug-resistant E. coli strain spreads through the so-called "fecal-oral route"—from feces to mouth, often via hands. Poor hand hygiene is one of the main reasons the bacterium spreads, but it can also be transmitted through food and water. Contaminated food, such as undercooked meat or vegetables washed in polluted water, are common sources of infection.
Good hand hygiene is essential to reduce the risk of infection. Regular handwashing with soap and water, especially after using the toilet and before preparing food, is the simplest and most effective way to stay healthy.
A major threat if the spread takes hold
Antibiotic resistance is one of the greatest health challenges we face today. When bacteria like E. coli become resistant, we lose the ability to treat common infections such as urinary tract infections or sepsis. This makes seemingly mild infections rapidly life-threatening.
The problem affects not only individuals but also entire healthcare systems. Without effective antibiotics, surgical procedures and cancer treatments become significantly riskier because there is no protection against infections. Minor illnesses that were once easily treated can lead to prolonged hospital stays, increased healthcare costs, and greater strain on healthcare resources.
If the spread of multidrug-resistant bacteria is not halted, we risk returning to a time when infections that are treatable today become fatal again. Preventing this requires both proactive measures and international collaboration to secure the future of public health.
According to the European Centre for Disease Prevention and Control (ECDC), the number of resistant infections in Europe has increased by over 30 percent in the last decade. Sweden has lower levels of resistance compared to many other countries but is not immune. The bacterium spreads freely between countries through travel, trade, and food.
Protect yourself by maintaining good hygiene
To protect yourself and reduce the spread, good hygiene is crucial. Wash your hands thoroughly and often, especially after using the toilet and before meals. When cooking, ensure meat is thoroughly cooked and vegetables are washed properly. Avoid unpasteurized products and refrain from drinking tap water when traveling to areas with known outbreaks.
Responsible use of antibiotics is also important. Only take antibiotics when necessary and as prescribed by a doctor to reduce the risk of resistance developing.
People in risk groups should take extra precautions
Although no one is entirely safe from this bacterium, certain groups are at higher risk of severe infections:
- Older adults with weakened immune systems.
- Patients with chronic diseases such as diabetes, kidney disease, or cancer.
- Recently operated patients or those receiving care in hospitals or nursing homes.
- Individuals with compromised immune systems due to illness or treatment, such as chemotherapy or immunosuppressive medications.
- Pregnant women who may be more susceptible to infections during pregnancy.
These groups are not only more likely to become infected but also have greater difficulty combating the infection without effective antibiotics.
How is E. coli identified?
To confirm an infection with the multidrug-resistant E. coli strain, laboratory tests are required. The diagnosis is made by identifying the bacteria in a sample from the infected body site, such as:
- Urine sample: For suspected urinary tract infection.
- Blood sample: If there are signs of sepsis.
- Stool sample: For suspected gastrointestinal infection or to locate the bacteria in the gut.
Once the bacteria have been isolated, they are analyzed to determine which antibiotics, if any, are effective. This is known as resistance testing and is crucial for selecting the right treatment.