Faecalibacterium prausnitzii
The gut flora is a complex ecosystem that plays a crucial role in our overall health. One of the most significant bacteria in this system is Faecalibacterium prausnitzii. This bacterium has been shown to offer several health benefits, including providing nourishment to the colonic mucosa, possessing anti-inflammatory properties, and improving insulin sensitivity. Let's delve deeper into the science behind these claims and how you can benefit your health by promoting this bacterium.
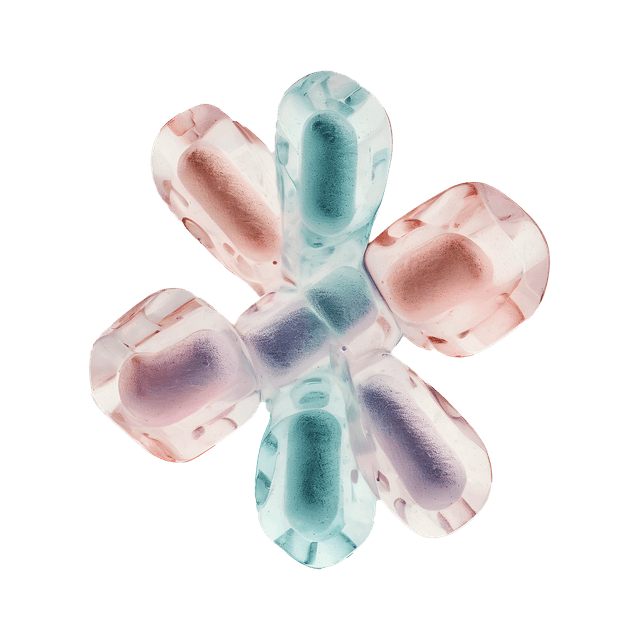
Nourishment for the colonic mucosa
Faecalibacterium prausnitzii produces butyrate, a short-chain fatty acid that serves as a key energy source for the cells of the colonic mucosa. A study published in FEMS Microbiology Letters demonstrates that this bacterium plays a central role in maintaining the integrity and function of the mucosa (1). Butyrate has also been shown to have anti-inflammatory properties, contributing to a healthy gut environment.
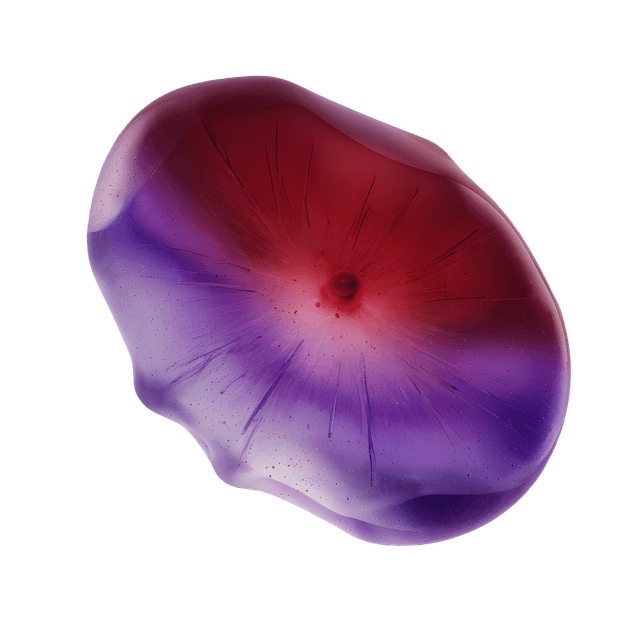
Anti-inflammatory properties
Inflammation is a natural part of the body’s defense system, but chronic inflammation can lead to several health issues. Faecalibacterium prausnitzii has been found to have powerful anti-inflammatory properties. A study published in Inflammatory Bowel Diseases found that low levels of this bacterium were associated with inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis (3). Increasing the levels of Faecalibacterium prausnitzii in the gut may potentially reduce inflammation and improve gut health.
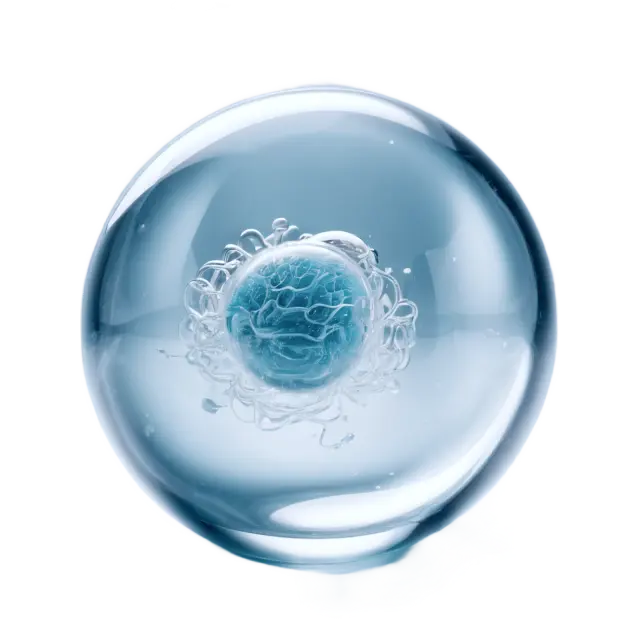
Reduced adipose tissue inflammation
Increased adipose tissue is often linked to low-grade inflammation, which can lead to metabolic diseases such as type 2 diabetes. A study published in Diabetes found that higher levels of Faecalibacterium prausnitzii were associated with reduced adipose tissue inflammation (4). This suggests that promoting this bacterium could potentially reduce the risk of metabolic diseases.
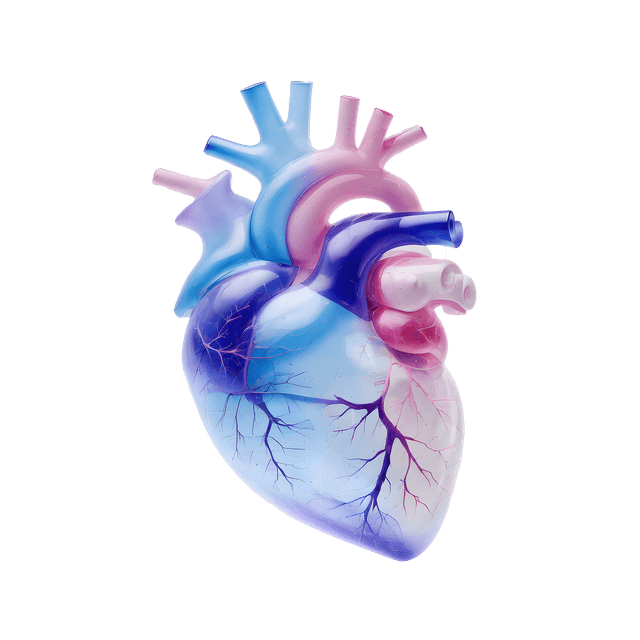
Improved insulin sensitivity
Insulin sensitivity is a crucial factor in maintaining blood sugar levels within a healthy range. A study published in Mediators of Inflammation showed that higher levels of Faecalibacterium prausnitzii were linked to increased insulin sensitivity in people with type 2 diabetes (5). This means that by increasing the amount of this bacterium, you could potentially reduce the need for insulin and improve blood sugar regulation.
How can you increase Faecalibacterium prausnitzii?
Here are some practical tips for promoting the growth of Faecalibacterium prausnitzii in your gut:
Eat Fiber-Rich Foods: Foods such as whole grains, fruits, and vegetables are high in fiber that acts as prebiotics, benefiting the growth of beneficial bacteria.
Probiotics: Although specific probiotic supplements with Faecalibacterium prausnitzii are not widely available yet, general probiotic supplements can help balance the gut microbiota.
Avoid Antibiotics: Antibiotics can eliminate both good and bad bacteria in the gut. Use them only when absolutely necessary.
Keep Stress Levels Low: Chronic stress can negatively affect the gut microbiota. Practice relaxation techniques such as meditation or yoga.
Conclusion
Faecalibacterium prausnitzii is a vital component of our gut microbiota with several health benefits, including nourishing the colonic mucosa, possessing anti-inflammatory properties, and improving insulin sensitivity. By following a few simple tips, you can help promote this beneficial bacterium and thereby enhance your overall health.
Scientific References
Petra Louis Harry J. Flint. Diversity, metabolism and microbial ecology of butyrate-producing bacteria from the human large intestine. FEMS Microbiology Letters, Volume 294, Issue 1, 1 May 2009, Pages 1–8.
Miquel S, Martín R, Rossi O, Bermúdez-Humarán LG, Chatel JM, Sokol H, Thomas M, Wells JM, Langella P. Faecalibacterium prausnitzii and human intestinal health. Curr Opin Microbiol. 2013 Jun;16(3):255-61.
Sokol H, Seksik P, Furet JP, Firmesse O, Nion-Larmurier I, Beaugerie L, Cosnes J, Corthier G, Marteau P, Doré J. Low counts of Faecalibacterium prausnitzii in colitis microbiota. Inflamm Bowel Dis. 2009 Aug;15(8):1183-9.
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, Mariat D, Corthier G, Doré J, Henegar C, Rizkalla S, Clément K. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010 Dec;59(12):3049-57.
Alessandra Puddu, Roberta Sanguineti, Fabrizio Montecucco, Giorgio Luciano Viviani. Evidence for the Gut Microbiota Short-Chain Fatty Acids as Key Pathophysiological Molecules Improving Diabetes. Mediators Inflamm. 2014; 2014: 162021. Published online 2014 Aug 17.