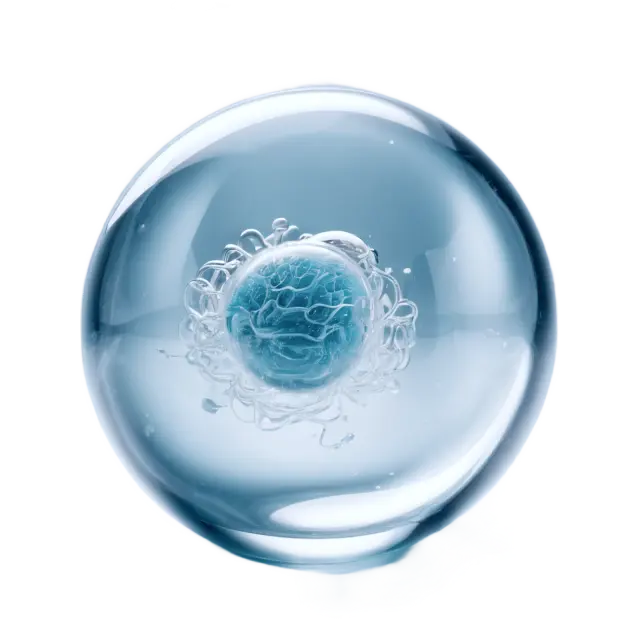
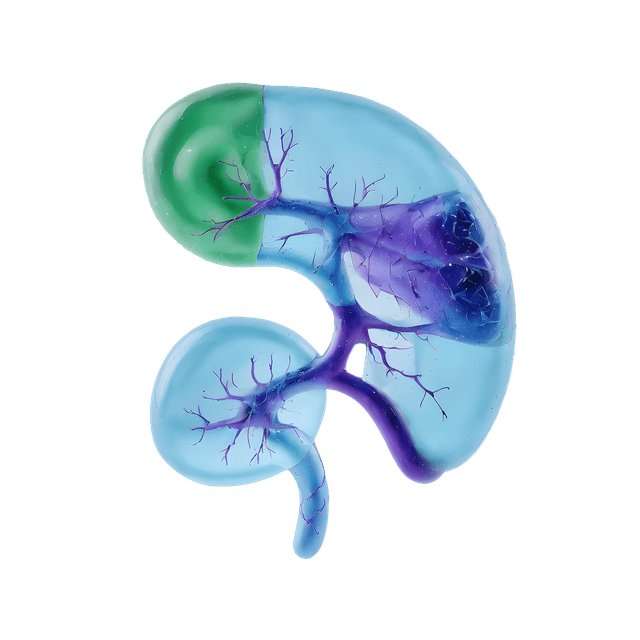
Insulin is a hormone produced by the beta cells of the pancreas. It is essential for regulating blood sugar levels by facilitating the uptake of glucose into cells. When we eat and blood sugar levels rise, the pancreas releases insulin to help cells absorb glucose and use it as energy.
What is the function of insulin in the body?
Insulin's primary function is to regulate blood sugar levels by assisting cells in absorbing glucose from the bloodstream. It also plays a key role in storing excess energy as glycogen and promoting fat storage and protein synthesis, which helps balance the body’s energy levels in both the short and long term.
- Regulation of blood sugar levels Insulin’s main task is to keep blood sugar levels within a healthy range. When we eat, carbohydrates break down into glucose, increasing blood sugar levels. Insulin helps cells absorb glucose from the blood, lowering blood sugar levels.
- Storage of excess energy In addition to regulating blood sugar, insulin helps store excess energy. When there is more glucose than the body needs for immediate energy, it is converted to glycogen, which is stored in the liver and muscles for later use.
- Fat and protein metabolism Insulin also plays a role in fat and protein metabolism by promoting fat storage and protein synthesis. This means insulin affects not only blood sugar but also the body’s overall energy balance.
What is insulin resistance?
Insulin resistance occurs when the body’s cells do not respond effectively to insulin, making it harder for glucose to be absorbed from the blood into the cells. In response, the pancreas produces more insulin to try to overcome the resistance, leading to higher levels of both insulin and glucose in the blood. Over time, this condition can impair the pancreas' ability to produce sufficient insulin, increasing the risk of developing type 2 diabetes.
Causes of insulin resistance
- Overweight and obesity Excess body weight, especially abdominal fat, is one of the main causes of insulin resistance.
- Physical inactivity Lack of exercise can gradually reduce the cells' sensitivity to insulin.
- Genetics Some people have a genetic predisposition to insulin resistance.
- Poor diet A diet high in sugar and refined carbohydrates can contribute to the development of insulin resistance over time.
Symptoms of insulin resistance
Insulin resistance often develops gradually, and many people notice no clear symptoms at first. However, as the body struggles to regulate blood sugar, certain signs may appear. Symptoms can vary depending on how long insulin resistance has been present and how much it affects the body. In some cases, the condition is only discovered when blood sugar levels become high enough to diagnose prediabetes or type 2 diabetes.
- Increased hunger, especially after carbohydrate-rich meals
- Fatigue and lack of energy
- Difficulty losing weight or unexplained weight gain
- Dark patches on the skin, especially in the armpits and neck (acanthosis nigricans)
- Increased thirst and frequent urination
- Difficulty with concentration and memory
Managing insulin resistance
Managing insulin resistance requires a combination of dietary and lifestyle changes. A healthy, fiber-rich diet with low sugar intake helps stabilize blood sugar and improves insulin sensitivity. Regular exercise, at least 150 minutes per week, helps muscles effectively use glucose without the need for extra insulin. Weight loss, even moderate, can significantly improve insulin sensitivity, especially in individuals who are overweight. Stress management through techniques like meditation or yoga is also important, as stress and high cortisol levels can worsen the body's response to insulin. Here’s a brief summary:
- Healthy diet
- Regular exercise
- Weight loss
- Stress management
Reference range for fasting insulin (Insulin FS)
The reference range for fasting insulin (Insulin FS) is generally