Causes Hyperlipidemia
Hyperlipidemia can be caused by several factors including heredity, diet, lifestyle choices, and disease. Here are some of the most common causes of hyperlipidemia:
Heredity: Genes play an important role in regulating cholesterol levels. Having a family history of hyperlipidemia or high cholesterol can increase the risk of developing the condition.
Diet: Excessive consumption of fatty foods, red meat and processed food can negatively affect lipid levels.
Lack of physical activity: A sedentary lifestyle can lead to obesity and high lipid levels. Regular physical activity can help regulate cholesterol levels.
Overweight and obesity: Obese people are at increased risk of hyperlipidemia especially if excess fat is stored in the abdomen .
Smoking: Smoking can lower levels of "good" HDL cholesterol and increase levels of "bad" LDL cholesterol which can increase the risk of hyperlipidemia.
Diabetes: People with diabetes often have higher triglyceride levels and lower HDL levels, which increases the risk of hyperlipidemia.
Alcohol intake: Excessive alcohol intake can increase triglyceride levels.
Some medications: Some medications including some diuretics, beta blockers, corticosteroids and some birth control pills, can affect lipid levels.
Diseases: Certain medical conditions such as hypothyroidism and kidney disease can affect lipid metabolism and lead to hyperlipidaemia.
Hormonal changes: Hormonal changes such as in menopause or during pregnancy can affect lipid levels.
It is important to understand that hyperlipidemia is often multifactorial and several of these factors can interact. The best way to manage hyperlipidemia is to adapt lifestyle and diet. In some cases, use medications under the supervision of a doctor.
Symptoms Hyperlipidemia
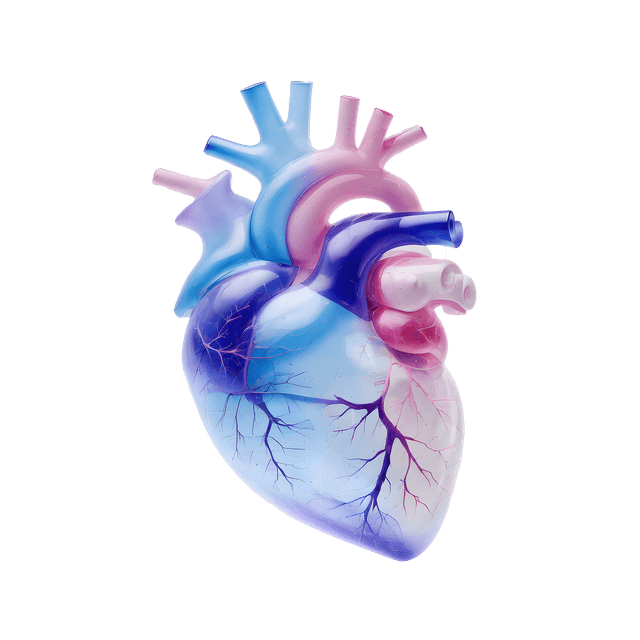
Hyperlipidemia is usually a silent condition, which means that it usually does not give rise to any immediately noticeable symptoms. Instead, the negative effects of high cholesterol levels and triglycerides manifest as complications such as cardiovascular diseases including atherosclerosis. The direct symptoms of hyperlipidemia are therefore usually indirect and related to the diseases that can develop. Here are some possible symptoms and signs:
Cardiovascular Disease: The primary threat of hyperlipidemia is its association with cardiovascular disease, including heart attacks and stroke. Symptoms may include chest pain (angina), irregular heartbeat and difficulty breathing.
Xanthelasma: This is a fatty deposit that can develop around the eyelids and is sometimes visible as yellow or white spots.
Xanthomas: This is another type of fatty deposit that can appear on tendons and joints leading to swelling and pain.
Vessel changes: Atherosclerosis, which is a common complication of hyperlipidemia, can lead to narrowing of the blood vessels. Symptoms that occur may depend on which arteries are affected and may include leg pain when walking or problems with blood flow to the brain.
Pancreatitis: Very high triglyceride levels can trigger inflammation of the pancreas which can cause severe abdominal pain, nausea and vomiting.
Jaundice: In rare cases very high triglyceride levels can cause jaundice which gives the skin a yellowish color.
It is important to note that most people with hyperlipidemia do not experience any of these symptoms until complications develop. Therefore, regular checks and blood tests to measure lipid levels are important to identify and manage hyperlipidemia at an early stage before serious health problems arise.
Treatment of Hyperlipidemia
The treatment of hyperlipidemia aims to lower high cholesterol and triglyceride levels to reduce the risk of cardiovascular disease. Treatment can include both lifestyle changes and medication, and the choice of treatment depends on the patient's lipid profile and individual risk factors. Here are some methods of treatment:
Lifestyle changes
Dietary changes: Reduce the intake of saturated fats, trans fats and cholesterol in the diet. Increase consumption of fiber-rich foods such as fruits, vegetables and whole grains. Fish rich in omega-3 fatty acids can be beneficial.
Exercise: Regular physical activity can help lower cholesterol levels. Recommended time for exercise varies but the goal is to get min 150 minutes of moderate intensity exercise per week.
Weight management: If overweight or obesity is a factor, weight loss through a healthy diet and exercise can help to lower lipid levels.
Quit smoking: Smoking can lower levels of the "good" HDL cholesterol. Quitting smoking is therefore an important measure for people with hyperlipidaemia.
Medication
Statins: Statins are common drugs that lower cholesterol levels by inhibiting the production of cholesterol in the liver. They include drugs such as simvastatin, atorvastatin, and rosuvastatin.
Fibrates: Fibrates are drugs primarily used to lower triglyceride levels and increase HDL levels.
Resins: Bile acid inhibitors or resins help reduce cholesterol levels by increasing the body's ability to remove cholesterol.
PCS9 inhibitors: PCS9 inhibitors are a newer type of medication that lowers cholesterol by increasing the liver's ability to clear cholesterol from the blood.
Some individuals may require a combination of different medications to achieve their lipid control goals. The treatment of hyperlipidemia should be individualized and supervised by a physician. Regular blood tests are important to evaluate the effectiveness of the treatment and adjust the medication if necessary.