What is testicular cancer?
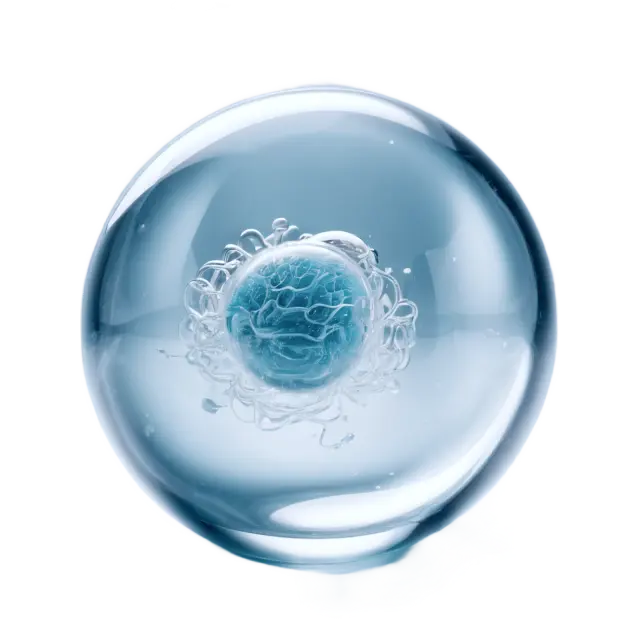
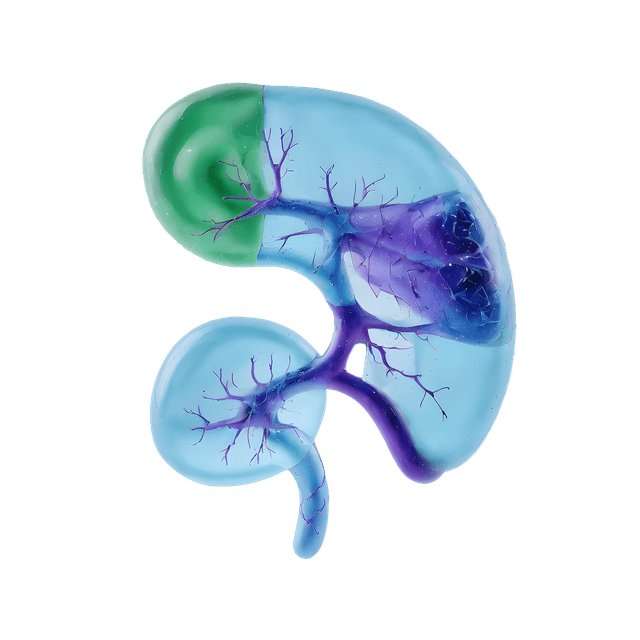
Testicular cancer arises in the testicles, where sperm and the male sex hormone testosterone are produced. There are two main types of testicular cancer:
- Seminoma – a slow-growing tumor that develops from germ cells in the seminiferous tubules of the testicles. It is sensitive to both radiation therapy and chemotherapy.
- Non-seminoma – a more heterogeneous group of testicular cancers that consist of different cell types, such as embryonal carcinoma, teratoma, choriocarcinoma, and yolk sac tumor. Non-seminomas tend to grow faster than seminomas and often require more intensive treatment.
Both types develop from the same type of germ cells but have different characteristics and treatment strategies.
Symptoms of testicular cancer
The most common symptom is an enlarged or swollen testicle. Other symptoms may include:
- A lump or hardness in the testicle
- Pain or discomfort in the testicle or scrotum
- A diffuse ache or heaviness in the scrotum
- Back pain or abdominal pain, if the cancer has spread to lymph nodes in the abdomen
- Breast enlargement (gynecomastia), which may be due to increased production of beta-hCG, a tumor marker
It is important to note that an enlarged testicle can also be due to other conditions, such as infection or fluid accumulation (hydrocele), which may require different treatment. Therefore, it is important to see a doctor if you notice any suspicious changes.
Diagnosis and examination
If a lump or induration is detected in the testicle, an ultrasound examination is usually performed to assess the structure of the tissue. Blood samples are also taken to analyze tumor markers, which can help determine the diagnosis and treatment strategy.
Tumor markers in testicular cancer
- AFP Alpha-1-Fetoprotein – Elevated in non-seminomas, but not in pure seminomas. A high AFP value means that the tumor contains non-seminomatous cell types.
- Beta-hCG HCG – May be elevated in both seminomas and non-seminomas. High levels of beta-hCG may indicate more aggressive disease, the same marker that is analyzed when pregnancy is suspected in women.
- LDH Lactate dehydrogenase – A less specific marker that may be elevated in more advanced testicular cancer and reflects the tumor burden.
If testicular cancer is suspected, the affected testicle is removed through an operation called an orchiectomy in order to confirm the diagnosis and analyze the type and spread of the tumor.
Treatment for testicular cancer
Treatment depends on the type of testicular cancer diagnosed and whether it has spread.
- Early-stage seminoma is treated with surgery and sometimes additional radiation therapy or low-dose chemotherapy to reduce the risk of recurrence.
- Non-seminoma is treated more often with cytostatics, especially if the cancer has spread. If the tumor is localized, surgery may sometimes be sufficient.
In disseminated disease, combinations of cytostatics are used, such as the BEP regimen (bleomycin, etoposide, and cisplatin), which has been shown to be very effective against testicular cancer. In some cases, surgery may be needed to remove metastases after cytostatic treatment.
Follow-up after treatment
After treatment has ended, patients are followed up regularly with blood tests and imaging tests (e.g., CT scan) to detect any recurrence at an early stage. Tumor markers such as AFP, beta-hCG, and LDH are measured at each follow-up to monitor whether the disease recurs.
Prognosis
The prognosis for testicular cancer is very good, especially if detected early. Approximately 98% of those diagnosed are completely cured, and even in the case of widespread disease, there are effective treatment options that can cure or significantly prolong survival.
Testicular self-examination
Regular self-examination can help detect changes early. This is easiest to do in the shower when the skin is relaxed:
- Feel each testicle with both hands and roll it gently between your thumb and fingers.
- Compare the testicles - it is normal for one to be slightly larger.
- Feel for lumps or calluses - even small changes should be examined by a doctor.
If you suspect changes, you should contact a doctor for further investigation.