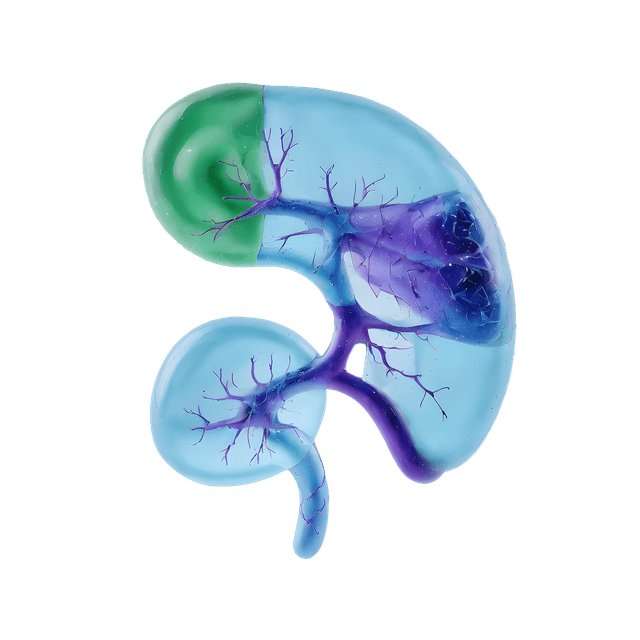
Prostatitis is an inflammation of the prostate gland that can be caused by various factors and affects men of all ages. The condition can be painful and impact both urinary and sexual functions, with symptoms that often vary depending on the type and severity. Some forms of prostatitis are short-term and easier to treat, while others may be chronic and require long-term management.
Types of prostatitis syndrome
-
Acute bacterial prostatitis
Caused by a bacterial infection, this is often a sudden and more severe form of prostatitis that requires immediate treatment. Symptoms can include fever, intense pain, and difficulty urinating. -
Chronic bacterial postatitis
A long-term bacterial infection in the prostate that may come and go over months or even years. Symptoms are usually less intense than those of acute bacterial prostatitis but can be challenging to fully resolve. -
Chronic rostatitis or (CPPS)
The most common form of prostatitis, where infection is not always involved. The cause is often unknown, but factors such as stress, muscle tension, or past infections may contribute to the symptoms. -
Asymptomatic inflammatory prostatitis
This form of prostatitis has no clear symptoms and is usually detected incidentally, for example, during a health check for other issues. Inflammation may, however, be indicated in laboratory tests.
Symptoms of prostatitis
The symptoms of prostatitis vary depending on the type of inflammation. Common signs to look out for include:
Pain or discomfort in the lower abdomen, groin, or lower back.
Difficulty urinating, frequent urination, or painful urination.
Sexual problems such as painful ejaculation or erectile difficulties.
Flu-like symptoms, such as fever and chills, particularly in cases of acute bacterial prostatitis.
Causes of prostatitis
The underlying causes and factors vary depending on the type of prostatitis. Acute bacterial prostatitis is usually due to bacterial infections that quickly produce symptoms and require immediate treatment. Chronic bacterial prostatitis involves a persistent infection that may recur despite treatment. Chronic non-bacterial prostatitis, also known as chronic pelvic pain syndrome (CPPS), is the most common form and often has unknown causes. It may be linked to factors like stress, previous infections, or muscle tension in the pelvic area. Although prostatitis can have several underlying factors, an accurate diagnosis is essential to ensure appropriate treatment and symptom relief.
Diagnosis and investigation in suspected prostatitis
Diagnosis of prostatitis involves a comprehensive medical history and symptom review to distinguish between different types of prostatitis. A digital rectal examination (DRE) is often performed to assess if the prostate is swollen, tender, or inflamed.
Further urine tests (sometimes including urine cultures) are analyzed to detect bacteria or signs of inflammation, especially if bacterial prostatitis is suspected. Blood tests may be conducted to measure inflammation markers, such as CRP, and occasionally PSA, as PSA levels can be elevated in cases of prostatitis.
PSA testing in prostatitis
PSA levels can be elevated in prostatitis due to inflammation, but the PSA test is primarily used for investigating prostate cancer and is not a routine part of prostatitis assessment. In some cases, PSA testing can still provide indications of the prostate's condition.
Treatment options
Treatment for prostatitis varies based on the type and severity of the condition:
Antibiotics: Mainly used for bacterial prostatitis.
Alpha-blockers: Help relax muscle tissue in the prostate and bladder neck, which can alleviate urinary symptoms.
Pain relievers: To reduce pain and discomfort.
Physical therapy: Can help with muscle relaxation and pain relief for chronic conditions.
Lifestyle changes: Regular exercise, stress management, and a healthy diet can have positive effects.
When to seek medical advice
If you experience symptoms of prostatitis, it is important to consult a healthcare provider for proper diagnosis and treatment. Ignoring symptoms may lead to complications, such as chronic pain or urinary tract infections.